Knowing when to test for COVID-19 can feel like a guessing game, but it boils down to a couple of straightforward rules. If you're showing symptoms, the answer is simple: test right away. If you know you've been exposed to someone who has it, the key is to wait 3 to 5 days before taking a test to get the most accurate result.
Your Quick Guide on When to Get a Covid Test
Figuring out the right moment to test is one of the most important things you can do to protect yourself and the people around you. With different types of tests and countless scenarios, it's no wonder people feel a bit lost. This guide is here to cut through the confusion and give you clear, practical answers.
Think of it this way: testing for COVID-19 too soon after an exposure is like checking on a cake you just put in the oven. All the ingredients are there, but they need time to actually bake into a cake. The virus works similarly—it needs time to multiply in your body before a test can detect it. Giving it a few days makes your test result far more reliable.
Common Testing Scenarios
To make things even clearer, let's walk through the most common situations where you might need a test. The flowchart below is a great visual starting point. It helps you quickly find your scenario—whether you're feeling sick, were recently exposed, or are just testing as a precaution—and shows you exactly what to do next.
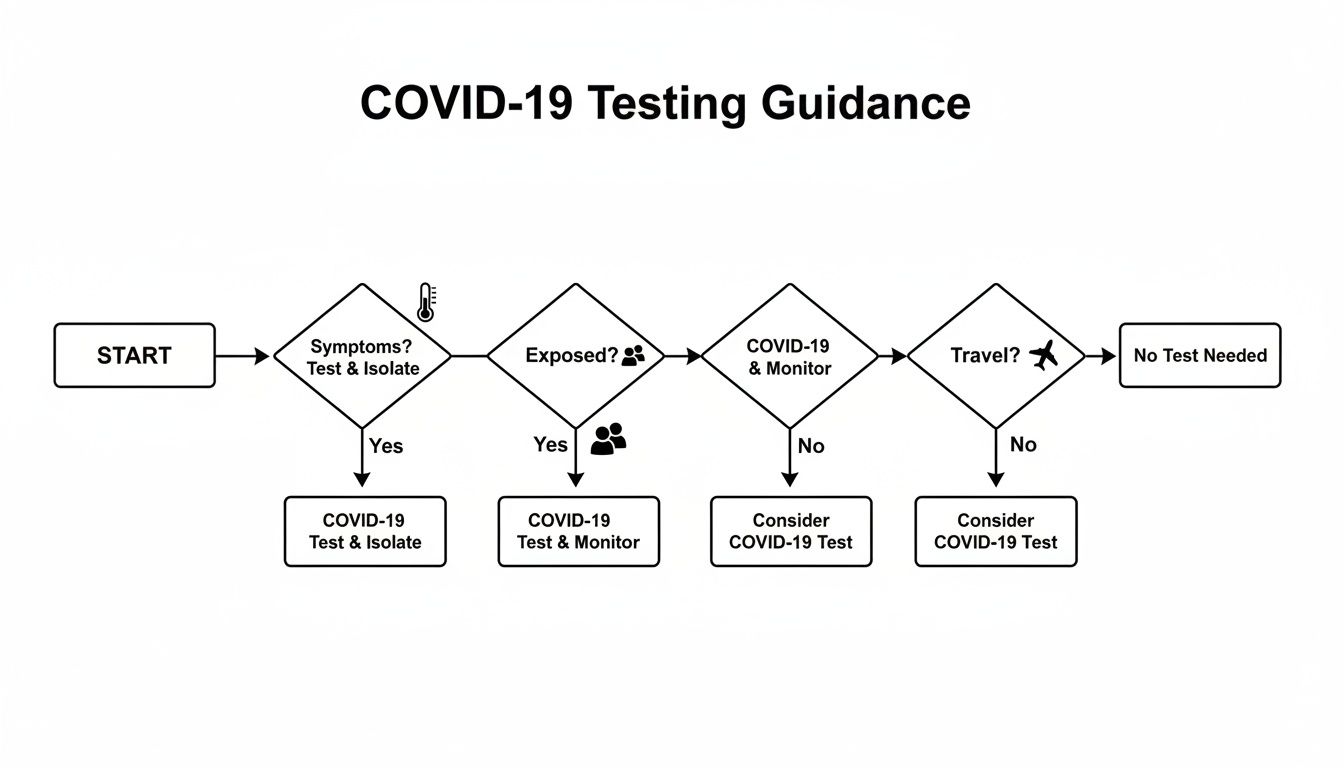
As you can see, the "why" behind your test—symptoms, a known exposure, or screening—is the biggest factor in determining your next steps. The chart gives you a simple path to follow for immediate guidance.
For an even faster breakdown, the table below is a handy cheat sheet. It lays out which test to grab and the best time to use it for each common situation.
Covid Testing At a Glance When and Which Test to Use
| Scenario | Recommended Test Type | Optimal Timing |
|---|---|---|
| You have COVID-19 symptoms | Antigen (Rapid) or PCR | Immediately when symptoms appear |
| You were exposed with no symptoms | Antigen (Rapid) or PCR | 3-5 days after last exposure |
| Pre-travel or event screening | PCR or Antigen (Rapid) | Check requirements; 1-3 days before event/travel |
| Ending isolation after infection | Antigen (Rapid) | Per guidelines, after symptoms improve |
Having this at your fingertips can help you make a quick, confident decision when you need it most.
Understanding the Two Main Types of COVID-19 Tests
To figure out when you should test, you first need to know what you’re testing with. It can feel a bit confusing with all the options out there, but it really boils down to two main players: PCR (Polymerase Chain Reaction) tests and Antigen tests, which you probably know as "rapid tests."
Think of them as two different tools for the same job. One is like a high-powered microscope, and the other is like a magnifying glass. Both can spot the virus, but they do it in very different ways, and each has its own strengths. Knowing which one to grab for your specific situation is the key to getting a reliable answer.
The PCR Test: The Gold Standard Detective
A PCR test is the forensic investigator of COVID tests. It isn't just looking for the virus; it's searching for its specific genetic fingerprint (the RNA). The lab takes your sample and uses a special process to make millions of copies of any viral RNA present, amplifying it until it’s impossible to miss.
Because of this amplification, PCR tests are incredibly sensitive and are considered the gold standard for accuracy. They can find even the smallest traces of the virus, which means they can often detect an infection earlier than other tests. It also means they can sometimes stay positive for weeks after you've recovered because they can pick up on leftover, non-infectious viral fragments.
The trade-off for this precision? Time. Your sample has to go to a lab, so you’ll usually wait a day or two—sometimes longer—for your result.
PCR tests are your best bet when you absolutely cannot be wrong. Think official travel requirements, pre-surgical screenings, or when you have symptoms but keep getting negative results on rapid tests and need a definitive answer.
The Antigen Test: The Fast and Practical Screener
If the PCR test is a forensic lab, the antigen test is like a quick field test. Instead of looking for genetic material, it hunts for proteins—called antigens—that sit on the surface of the virus. If enough of these proteins are in your nasal swab, you'll get a positive result.
The biggest win for antigen tests is speed. You get an answer right in your own home in as little as 15 to 30 minutes. This convenience is fantastic when you need a quick check before seeing family or if you wake up with a scratchy throat and just want to know.
But there’s a catch. For an antigen test to spot the virus, there needs to be a lot of it. This means they work best when your viral load is at its peak, which is usually a few days into having symptoms. If you test too early in an infection, you might not have enough virus for the test to detect, leading to a false negative.
When to Choose Each Test
So, how do you decide? It really comes down to a classic case of speed versus certainty.
Here’s a simple breakdown to help you choose the right tool for the job:
| Feature | PCR Test | Antigen (Rapid) Test |
|---|---|---|
| How it Works | Detects the virus's genetic code (RNA) | Detects proteins on the virus's surface |
| Best For | Unmatched accuracy and confirmation | Speed, convenience, and regular screening |
| Result Time | 1–3 days | 15–30 minutes |
| Sensitivity | Extremely high; finds tiny viral traces | Moderate; needs a higher viral load |
| Common Use | Confirming results, travel, medical needs | Testing when symptomatic, pre-event checks |
Ultimately, having both types of tests available gives you flexibility. If you feel sick and need an answer now, a rapid antigen test is a great first step. If you need absolute certainty for travel, work, or peace of mind after an exposure, the precision of a PCR test is the way to go.
The Best Time to Test After a Known Exposure
You just found out you were in close contact with someone who has COVID-19. Your first instinct is probably to grab a test and swab your nose right away. It’s a totally normal reaction, but acting on that impulse is one of the biggest mistakes you can make.
Testing too soon almost always leads to a false sense of security.
The reason is simple: it all comes down to the virus’s incubation period. Think of the virus like a seed that’s just been planted. It needs a few days to germinate and grow before any sprouts break through the soil. In the same way, the virus needs time to multiply in your body until it reaches a level that a test can actually pick up. This is what we call the viral load.
Testing on day one or two after you were exposed is like digging up that seed to see if it’s growing—you’re checking way too early and won’t find anything. Rushing to test often gives you an inaccurate false negative, where the test says you're clear even though an infection is quietly taking hold.
The Optimal 3-to-5 Day Testing Window
So, how long should you wait for a reliable result? Years of data have given us a clear sweet spot.
The most reliable time to test after a known exposure is three to five full days after your last contact with the infected person. This timing isn’t random; it’s based on giving the virus enough time to replicate to a detectable level.
By waiting at least three days, you dramatically increase the chances that your viral load will be high enough for either a PCR or a rapid antigen test to find it. A test taken inside this window gives you a much more trustworthy result.
This strategic waiting period became a key part of public health guidance. A major shift in understanding when to test happened when agencies started emphasizing post-exposure and post-travel testing to slow community spread. For example, on January 12, 2021, the CDC began requiring all air passengers entering the US to show a negative test before flying. Crucially, they also recommended that travelers test again 3-5 days after arrival. You can see a timeline of these public health milestones on the CDC's official website.
What to Do While You Wait to Test
That waiting period between exposure and your test is critical for protecting others. Just because you don't have a result doesn't mean you can't be contagious. It’s best to act as if you could be positive to keep those around you safe.
Here are a few practical steps to take while you wait for that optimal testing window:
- Monitor for Symptoms: Pay close attention to how you feel. Are you developing a sore throat, cough, fever, or unusual fatigue? The loss of taste or smell is another classic sign. If symptoms pop up, you should test immediately instead of waiting for the 3-5 day mark.
- Wear a High-Quality Mask: If you absolutely have to be around other people—even in your own home—a well-fitting N95 or KN95 mask is your best bet for preventing transmission.
- Limit Contact with Others: This is the time to hit pause on social plans. Avoid crowded indoor places, postpone gatherings, and work from home if you can.
- Inform Your Household: Give the people you live with a heads-up about your potential exposure. This allows them to take extra precautions, like wearing masks in shared spaces and opening windows for better ventilation.
Following these steps creates a buffer of safety for your community and helps ensure your test result is as accurate as it can be. It’s also a good idea to brush up on the difference between quarantine and isolation. For more on that, check out our resources for navigating COVID-19 isolation guidelines. This careful approach helps bridge the uncertain gap between exposure and a reliable test result.
What to Do When You Have Covid Symptoms
Waking up with that scratchy throat, a sudden fever, or a wave of exhaustion is a feeling we all know and dread. If you're experiencing symptoms that feel like COVID-19, the big question isn't if you should test—it's how soon you can. This is your cue to act fast.
Unlike testing after a possible exposure, where waiting is key, having symptoms changes the entire equation. Symptoms are your body's alarm bell, signaling that the virus is actively multiplying. This means your viral load—the amount of virus in your system—is probably high enough to be detected.
This is the perfect scenario for a rapid antigen test. These at-home kits are designed to pick up on viral proteins, and they're most accurate when there’s plenty of virus to find. Testing as soon as you feel sick gives you the best shot at an accurate positive result, so you can take steps to protect the people around you right away.

Why You Should Test Immediately with Symptoms
When you're sick, every hour counts. Putting off a test by a day or two might not seem like a big deal, but it can be the difference between isolating in time and accidentally spreading the virus further. The faster you know your status, the faster you can let close contacts know and start isolating.
This ability to test at home is a world away from the pandemic's early days. Back in early 2020, as the virus took hold in the U.S., testing was incredibly limited. Guidelines restricted tests to just three groups: recent travelers from outbreak areas, people sick enough to be hospitalized, or those who knew they'd been in close contact with a confirmed case. This piece of history really underscores why today’s guidance is so different—you don’t have to wait until you’re seriously ill. You can learn more about these early difficulties from the history of COVID-19 testing in the United States on Wikipedia.
When a Negative Rapid Test Isn't the Final Word
Okay, so you did the right thing. You took a rapid test as soon as symptoms popped up, but the result is negative. Is it time to celebrate? Not so fast. While a negative result is a good sign, it's not a guaranteed all-clear, especially if you still feel sick.
A negative rapid test while you have symptoms could mean a few things:
- You don't have COVID-19. Your symptoms might be from something else, like the flu or a common cold.
- Your viral load is still too low. It's possible you tested very early in your infection, before the virus had replicated enough for an antigen test to spot it.
- The test was a false negative. It happens. A poor swabbing technique or a faulty test kit can sometimes lead to an inaccurate result.
If your rapid antigen test comes back negative but you still have symptoms, the best next step is to get a PCR test. It’s considered the "gold standard" for a reason—it’s far more sensitive and can detect even tiny amounts of the virus, giving you a more definitive answer.
In the meantime, it’s smart to keep taking precautions. Isolate as much as you can and wear a good-quality mask if you have to be around others. At the end of the day, listening to your body is just as important as reading a test strip. And when you're feeling under the weather, it's always a good idea to focus on your body's natural defenses. For some tips, you might want to check out our guide on how to boost your immune system.
How to Use Testing for Travel and Social Gatherings

Testing for COVID-19 isn't just for when you feel sick or find out you've been exposed. It’s also an incredibly smart way to look out for others, especially before you head out on a trip or join a social event. This approach, often called screening, helps catch infections in people who feel perfectly fine, stopping the virus from spreading silently.
Think of it like checking the tire pressure on your car before a long road trip. You're not doing it because you have a flat tire; you're doing it to prevent a problem from happening down the road. That’s exactly what proactive testing does—it adds a vital layer of safety for everyone you’re about to see.
Navigating Rules for Formal Travel and Events
For formal travel and big, organized events, knowing when to test for COVID isn't just a good idea—it's often a strict requirement. Airlines, countries, cruise lines, and major venues can have their own set of rules you absolutely have to follow. Make sure you check the specific guidelines for your destination or event long before you plan to leave.
These rules are usually very specific. For instance, a country might require a negative PCR test taken no more than 72 hours before your flight departs. An antigen test might not cut it, and that timing window is firm. Get it wrong, and you could be turned away at the gate.
Here’s what you need to lock down before you go:
- Required Test Type: Do they need the high accuracy of a PCR test, or will a professionally administered antigen test do?
- Timing Window: This is critical. If the rule is 72 hours before departure, you have to schedule your test appointment to fall precisely within that timeframe.
- Proof of Result: What kind of documentation do you need? Will a digital result on your phone work, or do you need to bring an official, printed report from the lab?
Always go directly to the official government or event website for the latest info. These rules can and do change quickly.
Using Rapid Tests for Casual Social Gatherings
What about more casual get-togethers, like a family dinner, a birthday party, or visiting a relative who is more vulnerable? In these cases, the decision to test is up to you, and this is where at-home rapid antigen tests really shine. They may not be as sensitive as a PCR test, but their real power is speed.
The best time to take a rapid test for a social event is right before you leave the house. An antigen test gives you a snapshot of how infectious you are at that very moment, answering the question: "Do I have enough virus in my system right now to pass it to someone else?"
Testing a day or even a few hours ahead of time just isn't as reliable. Your viral load can shoot up fast, so a negative test on Friday morning doesn't guarantee you're still in the clear for a party on Saturday night.
Here’s a simple routine to make your gatherings safer:
- Test Just Before You Go: Swab and run your test within an hour or so of heading out the door.
- Stay Home if Positive: Any positive result—even a super faint line—means you need to cancel your plans and isolate. It's the only way to protect others.
- Encourage Others to Test: Gently suggesting that other guests do a quick test too can create a much safer space for everyone, particularly if older adults or immunocompromised friends will be there.
Interpreting Your Test Results and What to Do Next
Getting your test result is only half the battle. Knowing what it actually means for you—and the people around you—is what really counts.
Whether you see a positive or negative line, that result is a critical piece of information that dictates your next steps. Having a clear plan helps you move forward with confidence, making sure you take the right precautions at the right time.
Public health guidance has shifted quite a bit, and a key moment was back on June 13, 2020, when the CDC updated its guidelines, especially for high-risk settings like nursing homes. This just goes to show how important it is to not just get tested, but to know how to respond to the result you get. You can explore the timeline of COVID-19 testing on Wikipedia to see how recommendations have evolved.
What to Do After a Positive Test Result
Okay, so you tested positive. A positive result can feel a little jarring, but it gives you a clear and immediate mission: stop the spread. Your top priority is protecting others.
Here's exactly what you should do:
- Isolate Immediately: This is non-negotiable. Start separating yourself from others, even people in your own home. If you can, stick to a specific room and use a separate bathroom.
- Inform Your Close Contacts: Time to play detective. Think back to the 48 hours before your symptoms started (or before your test, if you have no symptoms). Anyone you were in close contact with needs a heads-up so they can take precautions and figure out when to test.
- Monitor Your Symptoms: Keep a close eye on how you're feeling. Track things like fever, cough, and fatigue. The good news is most people have a mild illness and can ride it out at home.
A positive test is a definitive sign you're infected and can pass the virus on. The single most important thing you can do is stay home and away from others to break that chain of transmission.
Understanding how long you're likely to be contagious is also crucial. For a detailed breakdown, check out our guide on how long COVID is contagious.
When to Contact a Doctor
While most infections are managed at home, you absolutely need to know the warning signs that mean it's time to get professional medical help.
Seek immediate medical attention if you experience any of these symptoms:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on your skin tone
These can be signs of a more severe illness that requires urgent care. Don't second-guess yourself—if you're worried about your symptoms, call your doctor or head to an emergency facility.
What to Do After a Negative Test Result
A negative result usually brings a wave of relief, but it isn't always a "get out of jail free" card. What it means really depends on your situation. If you have no symptoms and no known exposure, a negative result is pretty solid.
But what if you were recently exposed to someone with COVID-19? A negative test doesn't automatically give you the all-clear. It could be a false negative, especially if you tested too early (before that 3-to-5 day sweet spot). The virus might just not have built up to detectable levels yet.
If you test negative after a known exposure, you should still:
- Keep an eye out for symptoms for a full 10 days after you were last exposed.
- Wear a high-quality mask when you're around other people.
- Think about retesting in a day or two, particularly if you used a rapid antigen test.
This cautious approach prevents a premature negative test from giving you a false sense of security and accidentally spreading the virus.
Got Questions? We've Got Answers
Even when you know the basics, real-life situations with COVID testing can get tricky. It's one thing to know the rules of the road, but what happens when you hit an unexpected detour?
Think of this section as your personal troubleshooting guide. We'll walk through some of the most common and confusing questions to help you make the smartest health decisions with confidence.
When Should I Test After My Symptoms Go Away?
This is a big one, especially when you're trying to figure out if you can safely end isolation. The goal here isn't just to feel better, but to confirm you're no longer infectious to others.
For this specific job, a rapid antigen test is your best tool. A negative result is a good sign that your viral load—the amount of virus in your system—has dropped enough that you're not likely to spread it.
Most guidelines suggest you should be fever-free for at least 24 hours (without taking any fever-reducing medicine) and your other symptoms should be getting much better. For an extra layer of certainty, many experts recommend taking two rapid tests 48 hours apart. If both are negative, that's strong evidence you're in the clear.
Can I Really Trust a Negative Rapid Test?
This is a great question, and the answer is: it depends on the context.
A negative rapid test is pretty reliable if you have no symptoms and no known exposure. In that case, you can feel good about the result.
But the story changes if you're feeling sick or you know you were exposed.
- If you have symptoms: A negative rapid test might just mean your viral load is still too low for the test to pick it up. This is a classic "false negative" scenario. If you feel sick, the best move is to follow up with a PCR test to get a definitive answer.
- If you were exposed: Testing too early is a common mistake that gives people a false sense of security. You absolutely need to wait for that 3-5 day window after exposure. A negative test on day one or two doesn't mean much.
What if My Rapid Test Is Positive, But My PCR Is Negative?
Okay, this is a rare curveball, but it can definitely happen. While false positives on rapid tests are uncommon, they’re not impossible.
In this situation, you can generally trust the PCR test. PCRs are the gold standard for a reason—they are incredibly sensitive and accurate. A negative PCR result almost always overrides a positive rapid test, meaning you likely don't have an active COVID-19 infection.
That said, you shouldn't just leave it there. It's always a good idea to chat with your doctor. They can help you make sense of the conflicting results, look at your overall health, and make sure nothing else is going on.

