So, how long are you actually contagious with Covid? Let's get right to it.
You can typically start spreading the virus 1-2 days before you even feel sick, and you might remain contagious for up to 10 days. But the most important thing to remember is the peak window: you're most likely to pass it on to others within the first 5 days of showing symptoms.
Your Guide to the Covid Contagious Window

Figuring out exactly how long you're a risk to others is crucial for protecting the people around you. While that general timeline is a great starting point, the truth is, it’s not a simple one-size-fits-all answer. Your personal contagious window is shaped by a few key things, like when your symptoms pop up and how well your body is fighting off the actively replicating virus.
It's also really important to understand that testing positive doesn't automatically mean you're still contagious. A sensitive PCR test can pick up on tiny, non-infectious fragments of the virus for weeks after you’ve recovered and are no longer a threat to anyone. This guide is designed to give you a clear, practical roadmap to navigate all of this.
The Peak Contagious Period
Real-world evidence gives us a much clearer picture of when you're most likely to spread the virus. A groundbreaking study from Imperial College London found that the median duration of infectiousness was just five days.
Interestingly, even though many people tested positive before they felt sick, only about one in five was actually infectious during that pre-symptomatic phase. The study also showed that while two-thirds of people were still infectious five days after their symptoms started, their ability to transmit the virus dropped off a cliff after that.
This research drives home a critical point: The first five days of symptoms are, by far, the most important period for isolation. Your risk of passing the virus to someone else is at its absolute highest during this time.
To make this even clearer, the table below provides a quick summary of the typical contagious periods for different situations.
Covid-19 Contagious Periods At a Glance
| Infection Scenario | Typical Contagious Period | Peak Infectiousness |
|---|---|---|
| Symptomatic | Starts 1-2 days before symptoms, lasts up to 10 days. | The first 5 days after symptoms begin. |
| Asymptomatic | Shorter window; often ends around 7 days after a positive test. | Days 3-5 after initial viral detection. |
| Immunocompromised | Can be much longer; 20 days or more in some cases. | Varies greatly, may extend beyond the first week. |
Understanding these timelines helps you make informed decisions. It also underscores the value of maintaining simple daily health habits that keep your immune system in fighting shape. With this foundation, we can now dive deeper into the specifics for different scenarios.
The Science Behind How You Spread the Virus
To get a real handle on how long you're contagious with COVID-19, it helps to peek behind the curtain at what the virus is doing inside your body. Once SARS-CoV-2 gets in, it hijacks your cells and turns them into tiny virus-making machines. Their only job? Churn out millions of new copies of the virus.
This replication frenzy is what determines your viral load—a term that just means how much virus is actively circulating in your system. As those cellular factories ramp up, your viral load climbs. When your immune system starts shutting them down, it falls.
A higher viral load means you're breathing out more viral particles every time you talk, cough, or exhale. That’s what makes you more likely to infect someone else. Your level of contagiousness isn’t a simple on/off switch; it’s a curve that rises and falls right alongside your viral load. The entire time you're capable of spreading live, infectious virus is called your infectious period.
Why Viral Load Is Everything
Understanding viral load explains the most frustrating part of COVID-19: you can spread it before you even feel sick. In the one or two days before your first cough or fever, those viral factories are already working overtime. Your viral load is shooting up, often high enough to make you contagious even though you feel perfectly fine.
This pre-symptomatic window is a huge driver of transmission, simply because people are going about their daily lives, completely unaware they're spreading the virus.
Your viral load usually peaks within the first few days after symptoms start. This is when you're most contagious because the virus production is at its absolute highest. After that peak, your immune system finally starts getting the upper hand, dismantling the factories and causing your viral load to drop.
This predictable rise and fall is the reason public health guidance is structured the way it is. The initial five-day isolation period recommended by agencies like the CDC is designed to cover this peak infectious window when you pose the biggest risk to others.
Testing Positive vs. Actually Being Infectious
Here’s where things can get confusing: testing positive doesn't always mean you're actively contagious. This is where knowing the difference between the two main types of tests becomes incredibly useful.
-
Rapid Antigen Tests: These are basically "contagiousness" tests. They look for specific proteins on the surface of the virus, and they typically only turn positive when you have a high enough viral load to be shedding infectious particles. Think of them as a snapshot of your current risk to others.
-
PCR (Polymerase Chain Reaction) Tests: These are incredibly sensitive "detection" tests. They can find even the tiniest fragments of the virus's genetic material (RNA). While they're fantastic for diagnosing an infection, that same sensitivity can be misleading when you're trying to figure out if you're still a threat.
A PCR test can stay positive for weeks—or sometimes months—after you’ve fully recovered. It's not picking up live, dangerous virus. Instead, it's detecting harmless genetic leftovers, like finding rubble long after a building has been torn down.
This is a critical distinction. A lingering positive PCR test does not mean you can still infect people. On the other hand, a negative rapid test is a much more reliable sign that your viral load has dropped below the infectious level. Getting two negative rapid tests a day or two apart is an even stronger signal that it's safe to end isolation. Understanding this difference gives you the power to read your test results correctly and make smarter, more confident decisions.
A Day-by-Day Look at a Typical COVID-19 Infection
To really get a handle on how long you're contagious with COVID, it's helpful to walk through what a typical mild infection looks like from the moment you're exposed. Think of it as a roadmap of the virus's journey inside your body—it’s this timeline that forms the basis for public health advice.
The clock actually starts ticking well before you even feel a hint of sickness. This is what we call the presymptomatic phase.
The Presymptomatic Phase: The Sneaky Head Start
The virus doesn't politely wait for you to develop a cough or fever before it starts spreading. For about 1-2 days before any symptoms appear, your viral load—the amount of virus in your system—is already building up. You feel perfectly fine, but you can unknowingly pass the virus on to others.
This is a really critical window for transmission. We have solid epidemiological data confirming that people are infectious starting 1–2 days before symptoms show up and can stay that way for up to 10 days. In fact, research models suggest this silent, presymptomatic spread is responsible for a huge chunk of all transmissions, estimated at 37-43%. It's a major reason the virus moves so efficiently through communities. You can dig into the data yourself in the CDC analysis on COVID-19 transmission dynamics.
This hidden contagious window leads right into the period when you are most infectious.
The Peak Infectious Period: Days 1 to 5
Once symptoms kick in, your viral load usually hits its peak. The first five days of feeling sick are when you pose the biggest risk to others. During this time, your body is churning out the highest amount of virus, meaning you're shedding more of it every time you breathe, talk, or cough.
This is without a doubt the most important time to isolate yourself. Your ability to spread the virus is at its absolute highest, and even brief, casual contact can be enough to infect someone else.
The bottom line: The first five days of symptoms are the "danger zone" for spreading COVID. Your viral load is at its maximum, making this the time to be most careful. This is exactly why isolating during this period is so critical.
This timeline helps visualize how your viral load lines up with the infectious period and when a test is likely to turn positive.
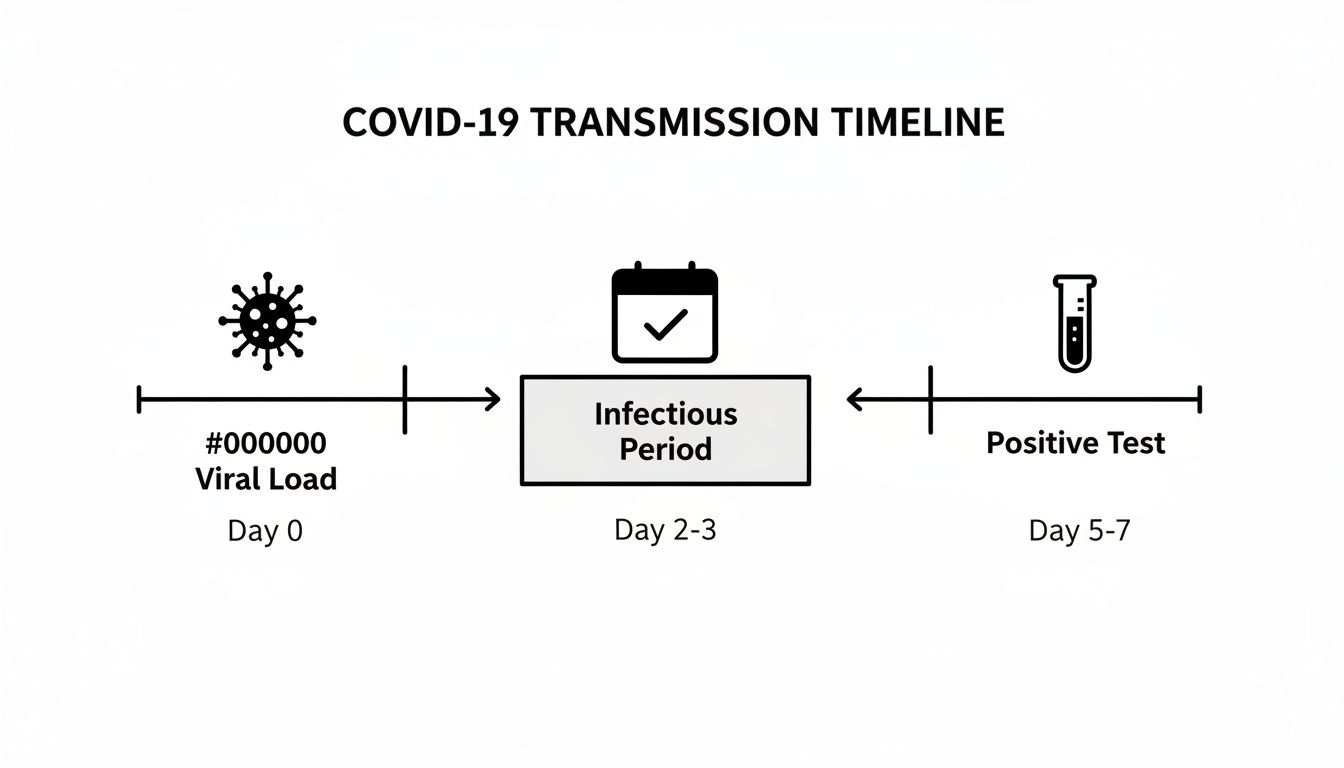
As you can see, you start being contagious before you're likely to test positive, and the risk is highest in those first few days after symptoms appear.
Winding Down: Days 6 to 10
After about day five, your immune system usually starts to get the upper hand. As it fights back and clears the infection, your viral load begins to drop—often quite steeply. As it falls, so does your ability to spread the virus.
You might still have some lingering symptoms, like a cough, but your risk of transmitting COVID-19 to someone else is much, much lower. For most people who had a mild or moderate case, the chance of being contagious is incredibly low by day 10.
Here’s a quick summary of that timeline:
- Days -2 to -1 (Presymptomatic): You feel fine but are becoming contagious as the virus multiplies.
- Days 0 to 5 (Symptomatic Peak): Symptoms arrive. Your viral load is at its highest, and you are most infectious.
- Days 6 to 10 (Declining Infectiousness): Your viral load drops sharply. You're far less likely to be contagious, especially by the end of this window.
Understanding this progression makes it clear why isolating early is so important. It also shows that just because you're starting to feel better doesn't mean you're immediately in the clear to be around others.
Factors That Can Change Your Contagious Period
While there’s a typical timeline for a COVID-19 infection, it's not a one-size-fits-all situation. Think of it more as a general blueprint. Your personal contagious window can actually stretch or shrink based on a few key factors.
Understanding these variables is crucial for making the safest decisions for yourself and the people around you. Just like a rainstorm can be anything from a light drizzle to a full-blown downpour, a COVID infection varies in intensity. The severity of your illness, the strength of your immune system, and your vaccination status all play a huge role.
Severity of Your Illness
It’s pretty simple: the sicker you are, the longer you’re likely to be contagious. A mild case is like a small brush fire that your body’s firefighters can quickly contain. Your viral load spikes early and then drops off fast, and you're often no longer infectious by day 10.
A severe case that lands you in the hospital, however, is more like a raging forest fire. The virus has more time and opportunity to replicate, leading to a much higher and more sustained viral load. It just takes the body longer to get things under control.
Studies have shown that while people with mild cases are rarely infectious after day 10, those with severe illness can shed the live virus for up to 20 days or even longer. For mild infections, the odds of still being able to spread the virus drop to just 6% by day 10, but that's not a reliable benchmark for more serious cases. To dig deeper into this, you can explore the research on contagious periods from the Global Virus Network.
Your Underlying Immune Status
How well your immune system functions is a game-changer. A healthy, robust immune system can launch a swift and powerful attack, shutting down viral replication and clearing the infection much faster. The result? A shorter contagious period.
On the flip side, someone who is immunocompromised has a much harder fight. This can be due to medical conditions like cancer, an organ transplant, or taking medications that suppress the immune system. Their body's defenses are quite literally handicapped.
Because their immune system can't clear the virus effectively, immunocompromised people can continue to shed infectious virus for weeks or even months. Their contagious window is often significantly longer, requiring extra precautions and guidance from a healthcare provider.
A strong immune response is your best line of defense. If you're looking for tips on keeping your body's natural defenses in top shape, check out our guide on how to boost your immune system.
Vaccination and Booster Status
Getting vaccinated is like giving your immune system the enemy's playbook before the battle even starts. It trains your body to recognize the SARS-CoV-2 virus and prepare a powerful counter-attack, which makes a huge difference if you end up with a breakthrough infection.
Research has consistently found that vaccinated and boosted people who get COVID tend to experience:
- Lower Peak Viral Loads: Their bodies get a head start on fighting the virus, keeping it from replicating to sky-high levels.
- Faster Viral Clearance: They successfully clear the virus out of their system more quickly than unvaccinated people.
- Shorter Contagious Periods: This powerful one-two punch of lower viral loads and faster clearance often means they’re contagious for less time.
So while vaccines don't always prevent an infection, they can seriously reduce your ability to pass the virus on to others, making them a vital tool for protecting the entire community.
The Specific Viral Variant
Finally, the virus itself matters. SARS-CoV-2 is constantly mutating, and different variants can have slightly different characteristics. For example, the variants circulating early in the pandemic seemed to have a longer contagious window.
More recent strains, like some of the Omicron subvariants, were found to have shorter incubation periods. This meant people got sick—and became contagious—much faster after they were exposed. While the core principle of isolating when you're sickest remains the same, these subtle shifts can tweak the average timeline by a day or two.
How Different Factors Affect Your Contagious Period
To put it all together, the contagious window isn't set in stone. The table below gives you a quick snapshot of how these different factors can either shorten or lengthen the time you're a risk to others.
| Factor | Impact on Contagious Period | Typical Duration |
|---|---|---|
| Mild-to-Moderate Illness | Standard duration of viral shedding. | Contagious period usually ends by Day 10. |
| Severe Illness | Higher viral load for longer; extends the infectious window. | Can be contagious for 20 days or more. |
| Immunocompromised Status | Impaired viral clearance leads to a much longer period of shedding. | May be contagious for weeks or even months. |
| Vaccination/Boosters | Faster immune response leads to quicker viral clearance. | Tends to shorten the standard contagious period. |
Ultimately, paying attention to these individual factors gives you a much clearer, more accurate picture of your personal risk and helps you make better decisions to protect those around you.
Making Sense of Public Health Guidelines
Trying to follow the official advice from public health groups can sometimes feel like you've been handed a map without a legend. But the guidelines from agencies like the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) aren't just random rules. They’re built directly on the science of how the virus behaves in your body.
Once you see how the recommendations line up with the timeline of your viral load, everything makes a lot more sense. Health experts pick a specific isolation period because it matches the window when you’re most likely to infect other people. Understanding that connection helps you move from just following rules to making truly informed decisions for yourself and those around you.
Let's break down the official guidance into clear, practical advice so you know exactly what to do.
The Logic Behind the 5-Day Isolation Rule
You've probably heard about the 5-day isolation period, which starts from the first day you feel sick. That number wasn't pulled out of a hat. It comes from a mountain of data showing that your viral load—and by extension, how contagious you are—hits its absolute peak during the first five days of symptoms.
By staying home during that critical window, you're essentially taking yourself out of the game when you pose the biggest threat. Think of it as creating a firebreak. You're stopping the blaze from spreading when it's burning hottest.
The goal of public health guidance is always harm reduction. Staying put for those first five days is the single best thing you can do to protect others, because it walls off the period when you're shedding the most virus.
After that initial five-day peak, your viral load usually starts to drop off a cliff. That’s why the guidelines often relax after day five—the risk of you passing the virus on is much, much lower.
What to Do After the Initial Isolation
The story doesn't end on day five. What you do next is just as important for catching any last bit of transmission. Here’s how to handle the days that follow:
-
Check Your Symptoms. Before you even think about leaving isolation, you need to be getting better. Your symptoms should be improving, and you must be fever-free for at least 24 hours without the help of medications like Tylenol or Advil. If you’re still feeling really sick on day six, you’re not ready—stay home.
-
Mask Up. Once you're out of isolation, wearing a high-quality, well-fitting mask around other people is non-negotiable. This recommendation typically extends through day 10. Think of the mask as your safety net, there to catch any lingering virus your body is still clearing out.
-
Protect the Vulnerable. Even with a mask, do your best to avoid close contact with people who are at high risk for severe COVID-19, like the elderly, people with weakened immune systems, or those with serious underlying health conditions. Your risk is low after day five, but it’s not zero.
This is a strategy of layered defense. Strict isolation tackles the peak risk, while careful masking and distancing handle the lower, tail-end risk. It’s a practical approach that balances protecting the community with letting people get back to their lives. When you connect these rules to the science, they become powerful tools you can use with confidence.
Using Tests to Know When You Are No Longer Contagious
While the official guidelines give us a solid timeframe for isolation, testing is the best way to get a personalized, real-world answer. It gives you the confidence to know you're not putting others at risk. The key, however, is knowing which test to use.
Using the wrong test can cause a lot of unnecessary confusion and keep you stuck at home longer than you need to be. The two main players—rapid antigen tests and PCR tests—have very different jobs, and understanding that difference is crucial.
The Rapid Antigen Test: Your Go-To for "Am I Still Infectious?"
Think of a rapid antigen test as a simple "Am I contagious right now?" test. It’s designed to hunt for specific viral proteins that are present when the virus is actively replicating in your body.
For a rapid test to turn positive, you generally need a pretty high viral load—which is exactly what makes you infectious to others. So, a positive result is a very clear signal that you can still pass the virus on.
This is what makes rapid tests the perfect tool for deciding when to end isolation. A negative result means your viral load has likely dropped below the infectious threshold.
But one negative test isn't always enough to be sure. For the highest level of confidence, experts point to the two-test strategy.
The Gold Standard for Ending Isolation: Once your symptoms are mostly gone and you’ve been fever-free for 24 hours without medication, take two rapid antigen tests spaced 48 hours apart. If both come back negative, you can be very certain that you're no longer contagious.
This approach confirms that your viral load isn't just low, but is staying down, giving you a much more reliable all-clear.
Why PCR Tests Can Be Misleading for Ending Isolation
On the flip side, PCR tests are the wrong tool for this specific job. They are incredibly sensitive, which makes them fantastic for diagnosing an initial infection. But that same sensitivity becomes a major drawback when you're trying to figure out if you're still contagious.
PCR tests can detect tiny, non-infectious fragments of the virus’s genetic material (RNA) long after you’ve recovered. It's like finding old footprints in the mud weeks after the person has walked away—the evidence is there, but the person is long gone.
Here’s why that’s a problem:
- Lingering Positives: You can continue to test positive on a PCR for weeks, and in some cases, even months after you're no longer infectious.
- Detecting "Viral Debris": A positive PCR result late in the game doesn't mean you're shedding live, transmissible virus. It's just picking up the leftover debris.
- Unnecessary Quarantine: If you wait for a negative PCR test, you could end up isolating for far longer than necessary, even when you pose zero risk to anyone around you.
So, when you're ready to see if you can safely re-enter the world, stick with the rapid antigen tests. They give you the real-time data you actually need.
Your COVID Contagiousness Questions, Answered
Even when you understand the science, real-life situations can still feel tricky. Let's walk through some of the most common questions people have about how long they're actually contagious.
If I Have No Symptoms but Test Positive, Am I Contagious?
Yes, absolutely. This is one of the toughest things about this virus—you can feel perfectly fine and still be contagious. It’s called asymptomatic transmission, and it’s a major reason COVID-19 has spread so widely.
A positive test means the virus is actively making copies of itself inside your body. Even without a single cough or sniffle, you can have a viral load just as high as someone who is sick in bed, especially during those first few days. That’s why following isolation guidelines is so important; you’re protecting others who might not handle the virus as well as you are.
Can I Still Be Contagious if My Symptoms Are Getting Better?
Yes, it’s entirely possible. Feeling better is a great sign—it means your immune system is doing its job! But contagiousness isn't about how you feel; it's about how much active virus you're still shedding.
Your symptoms can start to fade while your viral load is still high enough to infect someone else. This is precisely why health experts recommend isolating for a minimum of five days and then wearing a mask for several more. As your energy returns and your cough quiets down, you could still be shedding the virus. The best way to know for sure is to use a rapid antigen test to see if your viral load has dropped.
Does a Rebound Infection Make Me Contagious Again?
It sure does. If you experience a COVID-19 rebound—where symptoms come back or you test positive again just days after feeling better—you should consider yourself contagious all over again.
A rebound means the virus has managed to start replicating more aggressively, pushing your viral load back up into the infectious zone.
The CDC is clear on this: if you experience a rebound, you need to restart your isolation period from day one. Treat it like a brand-new infection to make sure you don't pass it on.
How Is Long COVID Related to Being Contagious?
This is a key point of confusion, but the answer is simple: Long COVID and being contagious are two totally different things. The contagious period is the short window—usually ending within about 10 days for most people—when you are actively shedding the live virus.
Long COVID, on the other hand, describes a whole host of health issues that can stick around for months or even years after the initial infection is long gone. These symptoms are thought to be caused by the body's prolonged reaction to the virus, like lingering inflammation, not by an ongoing, active infection. Someone with Long COVID is not contagious and poses no risk to others.
Focusing on your overall well-being is always a good strategy, and you can find more information in our articles on boosting immunity.
At The Happy Health Blog, we're committed to providing clear, reliable information to help you navigate your wellness journey. Explore our site for more expert-backed advice on nutrition, fitness, and balanced living. Find your path to a healthier life at https://thehappyhealthblog.com.

