It's important to understand that metabolic syndrome isn't a single disease. Instead, think of it as a cluster of five specific health markers that, when they show up together, act as your body's early warning system. Their combined presence dramatically increases your risk for developing serious, long-term health problems like heart disease, stroke, and type 2 diabetes.
Understanding This Cluster of Conditions
Imagine your body's health is like a symphony orchestra. For the music to be beautiful, every instrument has to be in tune. Metabolic syndrome is what happens when several key instruments—like your blood pressure, blood sugar, cholesterol, and body fat—are all playing out of tune at the same time. One off-key instrument might not ruin the whole performance, but a handful of them creates a cacophony that points to a much bigger problem.
This collection of risk factors has become incredibly common, largely driven by modern lifestyles that involve more sitting and more processed foods. The numbers are pretty staggering. In the United States, for example, nearly 40% of adults now meet the criteria. The risk also climbs with age, jumping from about 22% in young adults to over 56% for those 60 and older. Learn more about these global health trends.
Why It's More Than Just One Problem
The real danger of metabolic syndrome is its compounding effect. Each of the five markers—high blood pressure, high blood sugar, extra fat around the waist, high triglycerides, and low "good" HDL cholesterol—is a concern on its own. But when you have three or more, they start working together to accelerate damage throughout your body, especially to your heart and blood vessels.
This isn't just a list of unrelated issues; it's a connected web of metabolic dysfunction. Each factor can worsen the others, creating a feedback loop that dramatically elevates your long-term health risks.
This synergy is exactly why a diagnosis is so critical. It’s a crucial wake-up call, giving you a chance to make meaningful lifestyle changes before these risk factors snowball into more severe, life-threatening diseases.
To get a clear picture of what doctors are looking for, here's a quick reference guide to the five key health markers used to diagnose metabolic syndrome. A diagnosis is typically made when a person has at least three of these five conditions.
The Five Indicators of Metabolic Syndrome
| Health Marker | What It Measures | Threshold for Concern |
|---|---|---|
| Abdominal Obesity | The amount of visceral fat carried around your waist. | Waist circumference >40 inches (men) or >35 inches (women) |
| High Triglycerides | The level of a specific type of fat in your blood. | ≥150 mg/dL or on medication for high triglycerides |
| Low HDL Cholesterol | The level of "good" cholesterol that helps clear arteries. | <40 mg/dL (men) or <50 mg/dL (women) |
| High Blood Pressure | The force of blood pushing against your artery walls. | ≥130/85 mmHg or on medication for hypertension |
| High Fasting Glucose | The amount of sugar in your blood after not eating. | ≥100 mg/dL or on medication for high blood sugar |
Having just one of these markers is a reason to pay attention, but the real concern arises when they start to stack up. This table breaks down exactly what your clinician will be measuring.
Decoding the Five Key Markers of Metabolic Syndrome
To really get what metabolic syndrome is, you have to look at its five core components. A diagnosis isn't based on one single lab result; it's a combination of at least three of these distinct health markers. Each one tells a piece of the story about what's happening inside your body. Together, they paint a pretty clear picture of your overall metabolic health.
Think of them like the warning lights on your car's dashboard. One flashing icon might just be a heads-up for routine maintenance. But when three or more start blinking at once, it’s signaling a more serious problem that needs your immediate attention. Let's break down what each of these signals really means.
Marker 1: Central Obesity
The first marker is central obesity, which is just a technical term for excess fat stored around your middle. This isn’t about how you look—it’s about the type of fat. The stuff you can pinch on your belly (subcutaneous fat) is less of a concern than the deep, internal fat that pads your organs, known as visceral fat.
This visceral fat is surprisingly active. It pumps out inflammatory substances that can mess with your body's normal functions, including how it uses insulin. The clinical cutoffs are a waist circumference of 40 inches or more for men and 35 inches or more for women.
Marker 2: High Triglycerides
Next up, we look at triglycerides. These are a type of fat floating in your blood that your body uses for energy. When you eat more calories than you burn off, your body cleverly converts the extra into triglycerides and packs them away in fat cells for later.
Think of your bloodstream as a busy highway. A few triglyceride "trucks" are necessary to deliver energy, but too many create a massive traffic jam. A reading of 150 milligrams per deciliter (mg/dL) or higher, or being on medication to lower them, meets this criterion.
Marker 3: Low HDL Cholesterol
The third piece of the puzzle is low High-Density Lipoprotein (HDL) cholesterol. You’ve probably heard it called the "good" cholesterol, and for good reason. HDL acts like your body's cleanup crew. Its main job is to grab harmful cholesterol from your arteries and haul it back to the liver to be processed and removed.
If triglycerides are the cargo trucks clogging up the highway, HDL is the fleet of tow trucks keeping the lanes clear. When HDL levels are too low, you don't have enough of this protective cleanup crew on duty.
A level below 40 mg/dL for men or below 50 mg/dL for women is a major red flag for metabolic syndrome.
The connection between high triglycerides and low HDL is crucial. This combo doesn't just mean your blood is carrying too much fat—it also means your body can't clear it out effectively. It’s a one-two punch that can really accelerate damage to your arteries.
Marker 4: High Blood Pressure
High blood pressure, or hypertension, is the fourth marker. It's a measure of the force of blood pushing against your artery walls. When that pressure is consistently too high, it's like revving a car engine into the red for hours on end.
That constant force damages the delicate lining of your arteries, making them stiff and more prone to plaque buildup. It also makes your heart work way harder than it should have to, which over time raises your risk for a heart attack or stroke. The threshold here is a reading of 130/85 mmHg or higher, or being on medication for hypertension.
As you can see, these markers aren't just isolated numbers on a lab report. They are deeply interconnected factors that, when combined, create a direct pathway to serious chronic diseases like heart disease, stroke, and diabetes.
Marker 5: Elevated Fasting Blood Sugar
Finally, the fifth marker is elevated fasting blood glucose. This simple test measures the sugar in your blood after you haven't eaten overnight. High levels are a clear sign that your body is having trouble managing blood sugar, which is a classic symptom of insulin resistance.
When your cells start ignoring insulin—the hormone that acts like a key to let sugar in for energy—that sugar gets stuck in your bloodstream where it can cause all sorts of damage. A fasting blood glucose level of 100 mg/dL or higher, or taking medication for high blood sugar, completes the diagnostic picture.
The good news is that these markers often respond well to lifestyle changes. You can learn more about how to start exercising in our detailed guide.
Why Metabolic Syndrome Happens: Key Causes and Risk Factors
Metabolic syndrome isn't something you catch like a cold. Instead, it's a condition that creeps up over time as the body's finely-tuned systems start to go haywire. Think of it like an engine that's slowly falling out of tune. At the heart of this breakdown is one key problem: insulin resistance.
Here’s a simple way to picture it: Insulin acts like a key, unlocking your cells to allow glucose (sugar) in for energy. When you develop insulin resistance, it’s as if the locks on your cells get rusty. The key just doesn't work as well anymore.
To compensate, your pancreas goes into overdrive, pumping out more and more insulin to try and force those stubborn locks open. For a while, this brute-force approach works to keep your blood sugar in check. But it’s not a sustainable solution and creates a domino effect of other problems—the very issues that define metabolic syndrome.
The Role of Visceral Fat
So what causes our cells to become so "numb" to insulin in the first place? One of the biggest culprits is having too much visceral fat.
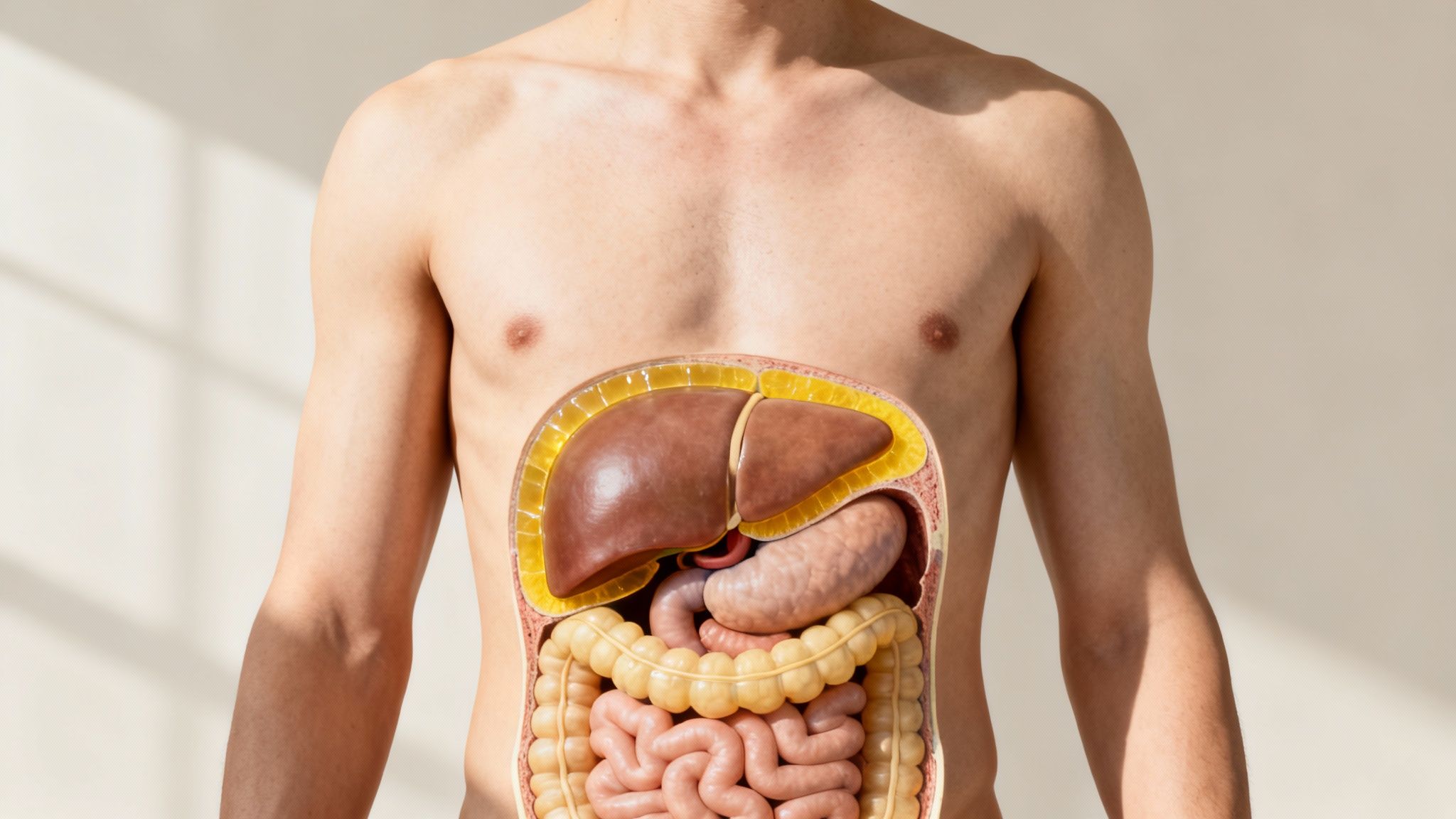
This isn't the fat you can pinch on your belly (that's subcutaneous fat). Visceral fat is the dangerous, hidden fat that wraps itself around your internal organs like the liver and intestines. It’s metabolically active, and not in a good way.
This internal fat acts like a toxic chemical plant, constantly releasing inflammatory signals and free fatty acids into your system. This chemical noise interferes with how insulin works, disrupting your body's hormonal balance and making your cells less responsive. This direct link is exactly why a large waistline is such a critical red flag for metabolic syndrome.
Key Drivers Behind Insulin Resistance
While insulin resistance is the central mechanism, a combination of factors determines who is most at risk. Some are out of your control, but many are not.
1. Genetics and Family History
Your DNA definitely plays a part. If you have close relatives with type 2 diabetes, high blood pressure, or heart disease, you may have a genetic predisposition that makes you more vulnerable to developing insulin resistance.
2. The Aging Process
The risk for metabolic syndrome naturally climbs as we get older. Most people lose muscle mass and gain body fat with age, a combo that can tank insulin sensitivity. Hormonal shifts, especially after menopause in women, can also change how and where the body stores fat, further complicating metabolic health.
3. Lifestyle and Environmental Factors
This is where you have the most influence. More often than not, our daily habits are the biggest drivers behind metabolic syndrome.
- A Sedentary Lifestyle: Not moving enough means your muscles don't need as much glucose, which contributes to weight gain and worsens insulin resistance.
- A Diet High in Processed Foods: Eating patterns heavy on refined sugars, unhealthy fats, and processed carbs flood your body with easy calories. This drives fat storage (especially that nasty visceral fat) and fuels chronic inflammation.
- Chronic Stress and Poor Sleep: Being constantly stressed out or sleep-deprived messes with hormones like cortisol. This can ramp up your appetite, encourage belly fat storage, and throw your blood sugar control completely off track.
The rise in metabolic syndrome closely tracks global shifts in how we live. One analysis found its prevalence jumped from around 15.5% in 2012 to 20.0% in 2021. The age-adjusted rate soared even more dramatically, from 12.8% to 20.8%, highlighting a serious public health trend.
These factors rarely work alone; they feed off each other. For instance, a diet filled with processed foods directly causes the kind of inflammation that disrupts your metabolism. This is why focusing on an eating plan rich in anti-inflammatory foods is so beneficial for your overall health. Understanding how these causes are interconnected is the first step toward taking control.
What Happens If Metabolic Syndrome Goes Unchecked?
Think of a metabolic syndrome diagnosis as a serious warning light on your car's dashboard. It’s not the breakdown itself, but it’s a clear signal that critical systems are under strain. Ignoring it doesn't make the problem go away; it just means a much bigger, more expensive, and more dangerous breakdown is coming. When the individual risk factors of metabolic syndrome team up, they don't just add to your health risks—they multiply them.
This isn't just a personal health issue; it's a global one with a staggering financial footprint. The economic weight of treating metabolic syndrome and the diseases it causes is immense. In fact, some analysts project the global market for related treatments could swell to between USD 100–150 billion by 2025, a direct reflection of its growing prevalence. You can dig deeper into these numbers in this detailed market analysis report.
The Fast Track to Type 2 Diabetes
Of all the potential consequences, type 2 diabetes is one of the most common and direct outcomes. The link is insulin resistance, the very heart of metabolic syndrome. For a while, often for years, your pancreas works furiously to pump out extra insulin to keep your blood sugar in check. But it's a battle it can't win forever.
Eventually, your pancreas becomes exhausted and can no longer produce enough insulin to overcome your body's resistance. That's the tipping point. Your blood sugar levels climb from the prediabetes range into a full-blown type 2 diabetes diagnosis. This isn't just about high blood sugar; it opens the door to a host of debilitating complications:
- Nerve damage (neuropathy), especially in the feet and hands
- Kidney disease (nephropathy) that can lead to dialysis
- Eye damage (retinopathy) that can cause vision loss and even blindness
- A significantly higher risk of infections and amputations
A Direct Assault on Your Heart and Blood Vessels
The other major threat is to your entire cardiovascular system. The dangerous trio of high blood pressure, elevated triglycerides, and low HDL cholesterol is the perfect recipe for damaging your heart and arteries. It’s a multi-pronged attack on the very plumbing that keeps you alive.
High blood pressure relentlessly hammers against your artery walls, causing them to become stiff, damaged, and less flexible. Meanwhile, the unhealthy cholesterol profile—too many triglycerides and not enough "good" HDL—promotes the buildup of sticky, fatty plaque inside those arteries. This process is known as atherosclerosis.
Imagine a pipe slowly getting clogged with gunk. Over time, the buildup narrows the passage, making it harder for blood to flow through. That's exactly what atherosclerosis does to your arteries, dramatically increasing your odds of a heart attack or a stroke.
The Ripple Effect on Other Organs
The damage doesn't stop there. The chronic, low-level inflammation and metabolic turmoil that define this condition can take a toll on other vital organs, too. A classic example is non-alcoholic fatty liver disease (NAFLD).
When your body is overloaded with fat and high triglycerides, it starts looking for new places to store them. Your liver is a prime target. Over time, this fat buildup can trigger inflammation and scarring (a condition called cirrhosis), crippling the liver's ability to do its many essential jobs.
Recognizing these risks is central to understanding why metabolic syndrome matters so much. But here’s the crucial takeaway: these serious outcomes are not inevitable. A diagnosis is your chance to change direction. It’s an urgent call to action, and responding to it is one of the most important things you can do for your long-term health.
Your Action Plan for Managing Metabolic Syndrome
Getting a diagnosis of metabolic syndrome can feel overwhelming, but it's better to see it for what it is: a powerful wake-up call. This is your body telling you it needs a change, and the most effective response starts with your daily habits. While medications can play a role, the foundation for reversing this condition lies in what you eat, how you move, and how you manage your life.
Think of it like getting a poor health report for the soil in your garden. You could use chemical fertilizers (medication) for a quick fix, but the real, long-term solution is to nourish the soil itself (your lifestyle). The best approach is to start improving the soil right away.

Fueling Your Body The Right Way
Good nutrition is where the magic happens. We’re not talking about a restrictive, temporary diet. The goal is a permanent shift to whole, unprocessed foods that help your body get back in balance.
The main focus is cutting back on processed junk loaded with sugar, unhealthy fats, and refined carbs, as these are major drivers of insulin resistance. Instead, you'll want to build your meals around real, nutrient-dense foods that keep your blood sugar stable. For a practical guide to making this switch, our clean eating meal plan is a great place to start, packed with simple tips and recipes.
Load your plate with these power players:
- High-Fiber Vegetables: Leafy greens, broccoli, and bell peppers slow down sugar absorption.
- Lean Proteins: Think chicken, fish, beans, and lentils. They keep you feeling full, which is a huge help for weight management.
- Healthy Fats: Avocados, nuts, seeds, and olive oil are your friends for improving cholesterol.
- Whole Grains: Quinoa, oats, and brown rice give you steady energy without the crash.
The Power of Purposeful Movement
Physical activity is a non-negotiable part of the plan. When you exercise, your cells become more receptive to insulin, which means your body doesn't have to work as hard to control blood sugar. It's also one of the best ways to burn dangerous visceral fat and improve blood pressure and cholesterol.
A great routine mixes both cardio and strength work. You don't have to become a marathoner overnight; consistency is what really matters here.
Aim for a weekly mix of:
- Aerobic Activity: At least 150 minutes of moderate-intensity exercise each week. This can be anything from a brisk walk or bike ride to swimming or dancing.
- Strength Training: Squeeze in at least two sessions a week that work your major muscle groups. Building muscle revs up your metabolism, as it burns more calories than fat, even when you're resting.
The best workout plan is the one you actually do. Start small. A 15-minute daily walk is a fantastic goal. Build from there and find activities you genuinely enjoy.
Sustainable Weight Management
You don't need to lose a dramatic amount of weight to see huge benefits. Losing just 5% to 10% of your body weight can dramatically improve all five markers of metabolic syndrome. For someone who weighs 200 pounds, that’s just 10 to 20 pounds.
Forget about crash diets; they're not built to last and can even backfire. The smart approach is a small, steady calorie deficit created by combining better eating habits with regular movement. This helps you lose fat while keeping your muscle, leading to real, lasting metabolic change.
To make this easier to digest, here's a quick look at the most impactful changes you can make.
Lifestyle Changes for Metabolic Health
| Lifestyle Area | Key Goal | Practical First Steps |
|---|---|---|
| Nutrition | Reduce processed foods, increase whole foods | Swap one sugary drink for water each day. Add a side of green vegetables to lunch and dinner. |
| Exercise | Increase daily movement and build muscle | Start with a 15-minute walk after dinner. Find a beginner's bodyweight strength routine online to do twice a week. |
| Weight Loss | Achieve a 5-10% reduction in body weight | Focus on your new eating and exercise habits; the weight loss will follow naturally. Avoid daily weigh-ins. |
| Stress | Lower chronic cortisol levels | Try 5 minutes of deep breathing exercises when you feel stressed. Take a short walk outside during your lunch break. |
| Sleep | Get 7-9 hours of quality, restorative sleep | Set a consistent bedtime. Turn off screens an hour before you plan to sleep. Make your bedroom dark and cool. |
Making these shifts consistently is the most powerful way to take back control of your metabolic health.
Beyond Diet and Exercise The Hidden Factors
Your action plan isn't complete without tackling two other critical pieces of the puzzle: stress and sleep.
-
Stress Management: Being chronically stressed means your body is constantly flooded with cortisol. This hormone can crank up your appetite (especially for junk food), tell your body to store more belly fat, and push your blood sugar up. Simple practices like mindfulness, yoga, or even just a few minutes of focused breathing can make a real difference.
-
Prioritizing Sleep: When you don't get enough quality sleep, the hormones that control your appetite go haywire, making you feel hungrier and crave unhealthy foods. It also makes it harder for your body to use insulin properly. Aim for 7-9 hours of solid sleep each night to give your body the rest it needs to heal.
The Role of Medication
Sometimes, even with dedicated lifestyle changes, one or more markers of metabolic syndrome might remain stubbornly high. If that's the case, your doctor might suggest medication to help get things back in a healthy range.
It's important to think of medication as a support tool, not a substitute for your healthy habits. It’s there to give your hard work an extra boost. Common prescriptions might help control blood pressure, manage cholesterol, or lower blood sugar. This is always a collaborative decision you'll make with your doctor based on your specific health needs.
When You Should Talk to Your Doctor
One of the trickiest things about metabolic syndrome is that it doesn't send up big red flares. It develops silently, so you can't rely on obvious symptoms to tell you something is wrong. That’s why being proactive and checking in with your doctor is one of the most powerful things you can do for your long-term health.
Regular check-ups are essential for everyone, but they become even more critical if you have known risk factors. If type 2 diabetes, high blood pressure, or heart disease run in your family, you'll want to be extra vigilant. It doesn't mean you're destined to have metabolic syndrome, but it does mean you should be more on top of preventive care.
Key Signs That Warrant a Visit
While metabolic syndrome itself is largely invisible, your body might still drop some clues that it’s time for a professional opinion. You should absolutely schedule an appointment if you notice:
- Your waistline is expanding: An increase in belly fat is one of the most visible signs. The benchmark to watch for is a waist circumference over 35 inches for women or 40 inches for men.
- You're constantly tired: Persistent fatigue that isn't solved by a good night's sleep can be a sign of insulin resistance. Your body is working overtime but struggling to use energy from food correctly.
- You're always thirsty or urinating more often: These are classic warning signs that your blood sugar might be creeping into the prediabetes or diabetes range.
What to Expect at Your Appointment
Your visit to the doctor will be a straightforward health assessment. The goal is to get a clear picture of your current metabolic health by measuring the five key components of the syndrome.
Here’s what you can generally expect:
- Physical Exam: Your doctor or nurse will measure your blood pressure and your waist circumference. Simple, quick, and painless.
- Blood Draw: You'll need a simple fasting blood test to check your glucose, triglyceride, and HDL cholesterol levels.
A diagnosis is not a life sentence—it's an opportunity. Getting your numbers gives you the power to team up with your doctor and make targeted changes that can genuinely protect your future.
Think of this visit as the start of a conversation. It's the first step toward creating a personalized action plan that puts you back in control of your health.
Answering Your Questions About Metabolic Syndrome
As you get to grips with what metabolic syndrome is and how to manage it, a few questions tend to pop up again and again. Let's tackle some of the most common ones to clear things up and help you move forward with confidence.
Can I Actually Reverse Metabolic Syndrome?
Yes, absolutely. For most people, reversing metabolic syndrome is a very achievable goal. Since the condition is almost entirely driven by lifestyle, making dedicated and consistent changes can bring all five of those key health markers back into a healthy range.
Think of it as turning off a series of warning lights on your body's dashboard. By sticking with healthier habits, you can normalize your blood pressure, blood sugar, cholesterol, and triglycerides while shedding that dangerous belly fat. It's not an overnight fix, but with sustained effort, you can completely turn the diagnosis around.
Is Metabolic Syndrome the Same Thing as Prediabetes?
That's a fantastic question, and while they aren't the same, they are very closely linked. Imagine two overlapping circles—that's the relationship between metabolic syndrome and prediabetes.
Prediabetes is a specific diagnosis: your blood sugar is higher than normal, but not quite high enough to be classified as type 2 diabetes.
Metabolic syndrome, on the other hand, is a much broader cluster of risk factors. High blood sugar is just one of the five possible criteria. Someone could technically have metabolic syndrome without prediabetes if their waist circumference, blood pressure, and cholesterol are out of line but their blood sugar is still in the normal range. Having metabolic syndrome, however, dramatically increases your chances of developing prediabetes and, ultimately, type 2 diabetes.
The most important thing to remember is that both conditions are a serious wake-up call. They’re a sign that your body’s metabolic health is under serious strain, and now is the perfect time to take action.
What’s the Single Most Important Change to Make?
If you're looking for the one thing with the biggest impact, the answer isn't a single action but a powerful combination: improving your diet and getting more physical activity at the same time. When you tackle both together, the effect is far greater than focusing on one alone.
A better diet helps reduce inflammation and manage calorie intake, while exercise is brilliant for making your cells more responsive to insulin and burning through harmful visceral fat. Focusing on these two cornerstones at once gives you the fastest, most sustainable path to reversing metabolic syndrome and protecting your long-term health.
At The Happy Health Blog, we're here to give you the guidance and motivation you need to make positive, lasting changes to your health. Explore our articles to take control of your wellness journey.

